Focus on gastrointestinal dysfunctions
R.E.D. Laboratories
Specialty Testing for Multifactorial Afflictions

+32.2.481.53.11
Who we are
R.E.D. Laboratories is private Belgian company developing tests for patients with complex clinical picture, chronic immune diseases and intestinal dysfunctions
We actively pursue new tests development in order to provide clinicians with updated tools
How we work
At R.E.D. Laboratories, we are continuously developing new tests according to the specific needs from health care providers.
All generated benefits are used for research and development of new assays.
We are involved in several international groups aiming to advance knowledge in biological markers of multifactorial afflictions that are not optimally supported by general health care systems.

Our philosophy
We focus on setting up the tests that are not (or rarely) available elsewhere.
Personalization of testing panel leads to more efficient and rapid management of patients with complex clinical picture.
Assay development programs at R.E.D. Laboratories focus on disorders that contribute to the onset and pathogenesis of diseases such as chronic fatigue syndrome, autism, chronic infections or autoimmune diseases.
What we offer
More and more evidence points towards a combination of factors (genetic, infectious, environmental, etc.) being important in the development of chronic immune dysfunctions, the cardinal finding in autistic, chronically infected and CFS patients.
In many countries these affections are still considered as psychiatric despite clear biomedical evidence.
For better management of these multifactorial affections suffering from lack of medical recognition, we offer SPECIALTY TESTS focused on 3 major topics:
Immune disorders,
Intestinal dysfunctions and
Infections
Check our website, our test request forms and our catalog for complete lists of tests and for newly available tests
Intestinal dysfunctions
Regulation of immune function in the gut
70% of our immune cells reside in the gut
Gut associated lymphoid tissue (GALT) is spread along the intestinal mucosa (Peyer’s patch in the small intestine, lymphoid follicles in the colon) and hosts 70% of the body’s immune cells
These immune cells permanently interact with mucosa-associated micro- organisms (bacteria, viruses…)
A delicate balance is maintained between tolerance to gut antigens (down- regulation of inflammation,…), and defense against pathogens (production of defensins,…)
Imbalance of gut immunity affects the whole body
Gut barrier integrity is essential :Increased permeability of the mucosa causes systemic endotoxemia (chronic low grade inflammation) and abnormal immune reactions to gut antigens
Interactions host/gut flora :the gut microbial flora plays a major role in maintenance of host health, but can be affected by abnormal host immune function

Establishment and composition of the gut flora
Human GI tract is colonized by 1014 microorganisms
Cytokines released by Th1 are: IL-2, IL-12, INFɣ, INFa and INFb
Colonization starts immediately at birth
Establishment of specific populations will depend on many factors, (normal birth or cesarean section, breast- vs formula feeding, hygiene conditions during the first months of life, early use of antibiotics, genetics…). At 1-2 years of age the ecosystem stabilizes.
Extreme diversity(500 to 1,000 different bacterial species)
Specificity: each individual displays a unique pattern of microbial diversity
Apparent stabilityover life, good resilience, but can be affected by drugs, infections, diet changes…
The microbiome contributes to the processing and metabolization of food
digestion and absorption of nutrients
sugar metabolism
synthesis of short chain fatty acids (eg, synth. of butyrate by Faecalibacterium, Roseburia… is important for colon health… but gives a lot of energy -> obesity)
synthesis of amino acids and vitamins (vit B12, vit B9, vit K)
detoxification of pollutants and toxic molecules present in the food
regulation of immune function


Testing offers at R.E.D. Laboratories intestinal dysfunctions
At R.E.D. Labs, we use the following assays to investigate intestinal dysfunctions:
Blood-based assays
sCD14 in serum
Lactase deficiency assay
D-lactate quantification in serum
Ammonia quantification in serum
Stool-based assays
sIgA ELISA test in stool samples
ZONULIN ELISA test in stool samples
EDN / EPX ELISA test in stool samples
Beta-Defensin-2 ELISA test in stool samples
Inflammation markers in stool samples
Infections in stool samples
MSA assay
Blood-based assays for intestinal dysfunctions
sCD14 in serumsCD14 is expressed in monocytes/macrophages and plays a critical role in the recognition of bacterial cell wall components (LPS). The extracellular part of CD14 can be cleaved and released in the plasma, where it will inactivate circulating LPS. Serum soluble CD14 levels are significantly elevated in patients with leaky gut, inflammatory bowel disease, Crohn’s disease, but also in patients suffering from Brucellosis or Lyme disease.
Lactase deficiency assay
a polymorphism in the gene coding for lactase, an enzyme responsible for the digestion of lactose (C/T- 13910 polymorphism). In affected people, production of the enzyme declines during or shortly after childhood, resulting in lactose malabsorption. Undigested lactose sugars affect the development of gut microflora, leading to dysbiosis.
D-lactate in serum
a product of bacterial metabolism, it is neither produced nor metabolized by mammalian cells. Typically, elevated D-lactate levels are due to bacterial infection or short bowel syndrome in humans. Due to slow metabolism and excretion, high D-lactate can cause acidosis and encephalopathy.
Ammonia in serum
Ammonia is derived from bacterial enzymatic action on ingested amino acids. It is absorbed from the gastrointestinal tract and delivered through the portal vein to the liver, which converts most of it into urea. Abnormally high levels of ammonia can result from colic or “enteric hyperammonemia” (combination of increased bacterial production and increased gut permeability) that occurs despite normal hepatic function. Hyperammonemia is a metabolic condition characterized by elevated levels of ammonia in the blood. Increased entry of ammonia to the brain is a primary cause of neurologic disorders, metabolic disorders and some toxic encephalopathies.


Stool-based assays for intestinal dysfunctions
sIgA ELISA test in stool samples
sIgA key function is to bind to invading micro organisms and toxins and entrap them in the mucus layer or within the epithelial cells, so inhibiting microbial motility, agglutinating the organisms and neutralizing their exotoxins and then assist in their harmless elimination from the body in the fecal flow.
The concentration of sIgA gives us information about the intestinal immune defense:
A lack of sIgAindicates a diminished activity of the intestinal immune system
An increased level of sIgA shows intestinal inflammation.
ZONULIN ELISA test in stool samples
Zonulin is the “doorway” to leaky Zonulin opens up the spaces between the cells of the intestinal lining. When leaky gut is present, the spaces between the cells open up too much allowing larger protein molecules and bacteria to get into the bloodstream where an immunologic reaction can take place. As the zonulin level rises, the seal between the intestinal cells diminishes. Zonulin is the only physiological modulator of intercellular tight junctions described so far that is involved in trafficking of macromolecules and, therefore, in tolerance/immune response balance.
beta-Defensin-2 ELISA test in stool samples
Defensins exert a variable degree of antimicrobial activity against bacteria, fungi, and some enveloped viruses. The expression of ß- defensins is induced by the pro-inflammatory cytokines and also through microorganisms (e.g. E. coli, H. pylori or P. aeruginosa) and by probiotic microorganisms. A ß-defensin-2 deficiency can, for example, be observed in the intestinal mucous of patients with Crohn’s The defense system of the mucous membrane is therefore restricted and allows an increased invasion of bacteria, which could possibly lead to a typical infection in Crohn’s disease patients. Recent results imply that ß-defensin-2 is overexpressed in active intestinal inflammation, especially in ulcerative colitis.


EDN / EPX ELISA test in stool samples
The accumulation of EDN in the intestine is associated with inflammation and tissue damage. Fecal EDN is considered the best of the cytotoxic granule proteins for assessment of gut inflammation. Elevated levels of fecal EDN are linked to multiple inflammatory conditions, like food allergy/sensitivity, pathogenic infections (C. difficile and Pylori), IBS, Eosinophilic Gastrointestinal Disorders.
Inflammation markers in stool samples
Hemoglobin: discharged with the feces in gastrointestinal bleeding diseases
Transferrin: a blood-derived component ; a good marker for gastrointestinal bleeding
Calprotectin: a neutrophil cytosolic protein with antimicrobial properties, which is present at increased concentration in stool during bowel inflammation
Lactoferrin: a primary component of the acute inflammatory response released from fecal leukocytes; may serve as a marker 1o2f inflammation in the intestine
Consequences of the leaky gut – chronic activation (inflammation) of the immune system
Lipopolysaccharide (LPS) – bacterial compound that can easily make its way to the blood.
Present in the bloodstream LPS will induce a strong pro-inflammatory response in monocytes and macrophages, involving recognition by a receptor (Toll-like receptor-4) and the subsequent secretion of cytokines such as IL-1, IL-6, TNF-alpha.
LPS also induces the NK-kB-mediated production of nitric oxide. Because NO is increased, NK function is inhibited and opportunistic infections such as mycoplasma infections are often observed.
Herpesviruses, which tend to reactivate in a context of immune activation, will also be frequently detected.

At R.E.D. Labs, these issues are evaluated by testing for
sCD14 expression
Cytokines’ expression
PGE2 expression
Virus detection in blood and intestinal biopsies
Mycoplasma infections
Oxydative stress
Testing offers at R.E.D. Laboratories intestinal dysfunctions
Stool-based assays
Infections assessments in stool samples


Metagenomic stool assay (MSA)
Intestinal microbiota analysis : from culture to high-throughput sequencing:
Until recently research into microbiota composition relied almost exclusively on culture ; 40 to 80% of gut bacteria cannot be cultured.
Identification of colonies can be difficult
Bacteria must be alive: studies of anaerobes very difficult, major loss during collection and processing of samples
Culture approach may address only a small fraction of all bacterial species (10%?)
E.coli once thought to be a dominant species, is a minor member…
R.E.D. Labs scientists have developed and validated a new procedure to analyze bacterial populations in a stool sample : MSA assay
New molecular technique involving sequencing of specific regions of bacterial DNA (metagenomics)
Can be performed on dead organisms (exposure to oxygen, freezing are not a problem)
Identification of each bacteria by comparing sequence with public databases: extremely precise, not subjective
High-throughput technology allows identification of tens or even hundreds of thousends organisms in a single sample
Bacterial DNA was extracted from stool samples, PCR amplification was performed on 16S rRNA gene regions, and PCR amplicons were sequenced Bacteria were classified b1y5 phylum, family and genus

MSA assay template report

MSA assay template report

Signs and symptoms related to the gastrointestinal tract and liver may provide important clues for the diagnosis of various tickborne diseases
FROM: GASTROINTESTINAL AND HEPATIC MANIFESTATIONS OF TICKBORNE DISEASES IN THE UNITED STATES SYED ALI ZAIDI & CAROL SINGER, CLIN INFECT DIS. 2002;34(9):1206-1212. DOI:10.1086/339871

Lyme disease and gastrointestinal disorders
Patients with Lyme and TBDs may present primarily with GI
2015 ILADS conference, Farshid Rahbar: These patients may have complex or persistent GI symptoms involving upper, mid, or lower GI tract and have already been treated for GI issues
Bloating/Gas: in 76% of patients
Abdominal Pain: in 48% of patients
Constipation: in 42% of patients
Food Intolerance: in 42% of patients
Irregular Bowel Movements: in 37% of patients
The number of patients presenting with such symptoms is probably reaching epidemic proportions.
Testing for gastrointestinal problems need to be included
Useful assays to investigate intestinal dysfunctions:
BLOOD-BASED Tests: Ammonia in serum, Lactase deficiency assay, D-lactate, sCD14
BIOPSY-BASED Tests: PCR-based detection of viral and bacterial infections
STOOL-BASED Tests:
Intestinal Inflammation: sIgA, Beta-2 Defensin, EPX / EDN, Inflammation markers in stool samples
Intestinal Infections : immunochromatography antigenic testing for intestinal infections
Leaky gut: ZONULIN ELISA test in stool samples
Dysbiosis: MSA assay (metagenomic stool test)

Consequences of TBI

Although ASD primarily impacts the brain, over recent years, links with other systems have become clear — in particular, gastrointestinal (GI) issues seem to occur more often in individuals with ASD than in the rest of the population.
The GI issues that come with ASD might be due to two factors: firstly, inappropriate immune activation, causing inflammation of the tract; and, secondly, differences in the types of gut bacteria that are present.
Gut-brain axis in autism

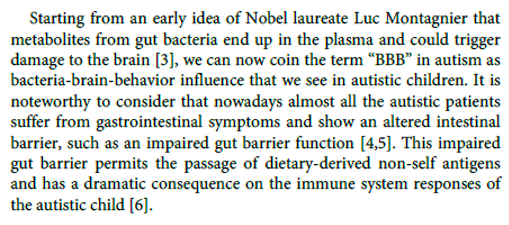

Intestinal dysfunctions in autism
Gut flora and gastrointestinal status in children with autism correlate with autism severity
of beneficial bacteria that were investigated, the children with autism had much lower levels of Bifidobacterium (-45%), slightly lower levels of Enterococcus (-16%), and much higher levels of Lactobacillus (+100%).
Finegold et al. (Anaerobe 2010) reported that in the control children’s stools, Firmicutes accounted for 63.6% of the total flora but only 38-39% of the flora of autistic children’s stools. Bacteroidetes accounted for 30% of the stool flora in controls and for 51% in the flora of stools of autistic children. Actinobacteria made up 1.8% of stool flora of control children and between 0.4 and 0.7% of the flora of autistic children. Proteobacteria made up 5% of the flora of control children and between 2.3 and 3.1% of the flora of autistic children. In summary, the fecal flora of autistic children was statistically significantly different from the fecal flora of healthy children.
R.E.D. Laboratories are offering specialty test to deeply analyze gut microbiota: MSA assay
ASD Child MSA
ASD Child MSA
Prevotella: strong hydrogen sulfide (H2S) producers. In excess, H2S acts as a mitochondrial poison and a potent neurotoxin. It can directly inhibit enzymes involved in the cellular production of energy. H2S also interferes with oxygen transport by blocking hemoglobin in the red blood cells. Finally, H2S is lowering gut pH preventing the growth of many beneficial bacteria,


ASD Child MSA
1st visit April 2017:
High both Bacteroides & Prevotella
2nd visit December 2017: Still high Bacteroides but normalized Prevotella
3rd visit December 2018: Normalized both Bacteroides and Prevotella
ASD adult 28y Streptococcus:
interact with the part of the brain known as the basal ganglia. This is believed to cause the sudden onset of tics or obsessive compulsive behaviors.


Intestinal inflammation in autism
Autism and gastrointestinal inflammation
Several reports have revealed a high prevalence of gastrointestinal symptoms, inflammation, and dysfunction in children with autism (reviewed by Horvath and Perman, Curr Gastroenterol 2002).
Mild to moderate degrees of inflammation were found in both the upper and lower intestinal tract. In children with ASD, the presence of GI dysfunction is often associated with increased irritability, tantrums, aggressive behavior, and sleep disturbances (reviewed by Critchfield et al., Gastroenterol Res 2011).
Leaky gut in ASD children

CFS-related disorders subgroups: intestinal dysfunctions
Evidence for GI dysfunction in CFS (Chronic Fatigue Syndrome)
Gastro-intestinal symptoms in patients
More than 90% of CFS patients will present IBS symptoms during their life
co-occurrence of CFS and IBS is associated with increased levels of inflammatory cytokines [Aaron et al., Arch Internal Med 2000; Scully et al., Am J Gastroenterol 2010]
Endoscopic evidence
Endoscopic examination of duodenum or stomach almost systematically reveal the existence of inflammed areas of the mucosa
Inflammatory markers in stools


CFS-related disorders subgroups:intestinal dysfunctions
Dysbiosis in CFS
A frequent disorder of intestinal function is dysbiosis, i.e. the overgrowth of pathogenic bacteria in the intestine.
Several published studies suggest that CFS is associated with dysbiosis
Culture-based assays revealed increased levels of Streptococcus and Enterococcus spp. in faecal samples of ME/CFS patients [Sheedy et al., In Vivo 2009]
Probiotic supplementation( casei in one study, L. paracasei + L. acidophilus + B. lactis in another study) resulted in improved emotional symptoms and neurocognitive functions [Rao et al., Gut Pathog 2009; Sullivan et al., Nutr J 2009]
We use the following assays to investigate intestinal dysfunctions:
sCD14
Lactase deficiency assay
sIgA ELISA tests in stool samples
Zonulin ELISA tests in stool samples
Beta-2 defensin ELISA tests in stool samples
EPX / EDN ELISA tests in stool samples
Inflammation markers in stool samples
MSA assay
PCR-based detection of viral infections


Viral infections : Several viruses have been associated with CFS
Human Herpesvirus 6 and 7 [Chapenko et al., J Clin Virol 2006]
Enteroviruses [Chia et al., J Clin Pathol 2010]
Parvovirus B19 [Kerr et al., J Gen Virol 2010]
Bornavirus [Nakaya et al., FEBS Lett 1996]
Epstein-Barr virus [Lerner et al., In Vivo 2004]
Not specific for CFS; none of these viruses found in all CFS patients
Persistent viral infections can affect intestinal immunity
HHV-6 is immunosuppressive, causes depletion of CD4 cells, down-regulation of CD3 in infected T cells, alteration of cytokine expression (TNFa, IL-1b, IL-10, IL-12). Parvovirus infection associated with altered IFNg response.
Consequences on intestinal health
Immunosuppression may favor development of other viruses or pathogens; alteration of gut immunity can also affect the gut flora
Viral infections: Search for viruses in the gut mucosa: rationale and experimental approach
The gastro-intestinal mucosa is a known reservoir for several viruses
HHV-6, HHV-7, CMV are found in intestinal biopsies of HIV patients and transplant recipients;
EBV is found in the gastric mucosa, associated with gastritis and gastric cancer; chronic
enteroviral infections have been found in the stomach of CFS patients
A study has been conducted at RED Laboratories to investigate the presence of specific viral infections in the GI tract of CFS patients
Experimental approach
Determination of HHV-6, EBV and parvovirus B19 viral loads in gastric and intestinal biopsies of CFS patients and non-CFS controls, by real-time quantitative PCR. 48 patients, 35 controls.
PUBLISHED IN: IN VIVO 2009; MAR-APR;23(2):209-13.DETECTION OF HERPESVIRUSES AND PARVOVIRUS B19 IN GASTRIC AND INTESTINAL MUCOSA OF CHRONIC FATIGUE SYNDROME PATIENTS. BY FRÉMONT M, METZGER K, RADY H, HULSTAERT J, DE MEIRLEIR K.


Viral infections : HHV-6 viral loads in positive biopsies
Several highly positives in the gastric mucosa of CF
Higher loads in stomach than in doudenom.
Viral infections : Parvovirus B19 in stomach and duodenum biopsies

Frémont et al., In vivo 2009
Higher frequency of Parvovirus B19 in both gastric and duodenal mucosa of patients compared to controls
Questions and contacts
References: FT-Mijatovic-red-labs-presentation-gastro-2021
Material available on the website ( redlabs.com)
Check regularly our website (www.redlabs.com) for the updates
Questions and contact:
General queries, logistics : E-mail to info@redlabs.be
Scientific questions : E-mail to tmijatovic@redlabs.be






